Progress does not stop with age: how to train for life
Age-related declines in physical fitness and health are not a sure thing — here's how you can subvert expectations and stay fit as you grow older.
Jun 1, 2021Mathew Welch, ATC, CSCS
May 26, 2023 | Elisa LaBelle, PT, MSPT

“Oh yeah? Well, just wait until you’re my age…”
“That routine won’t work for someone in their 50s.”
“This is what happens! As you get older, things start to break down.”
- How many times have you been told this from a friend, colleague or worse, a fitness or healthcare professional? Here are some cold, hard stats that matter:
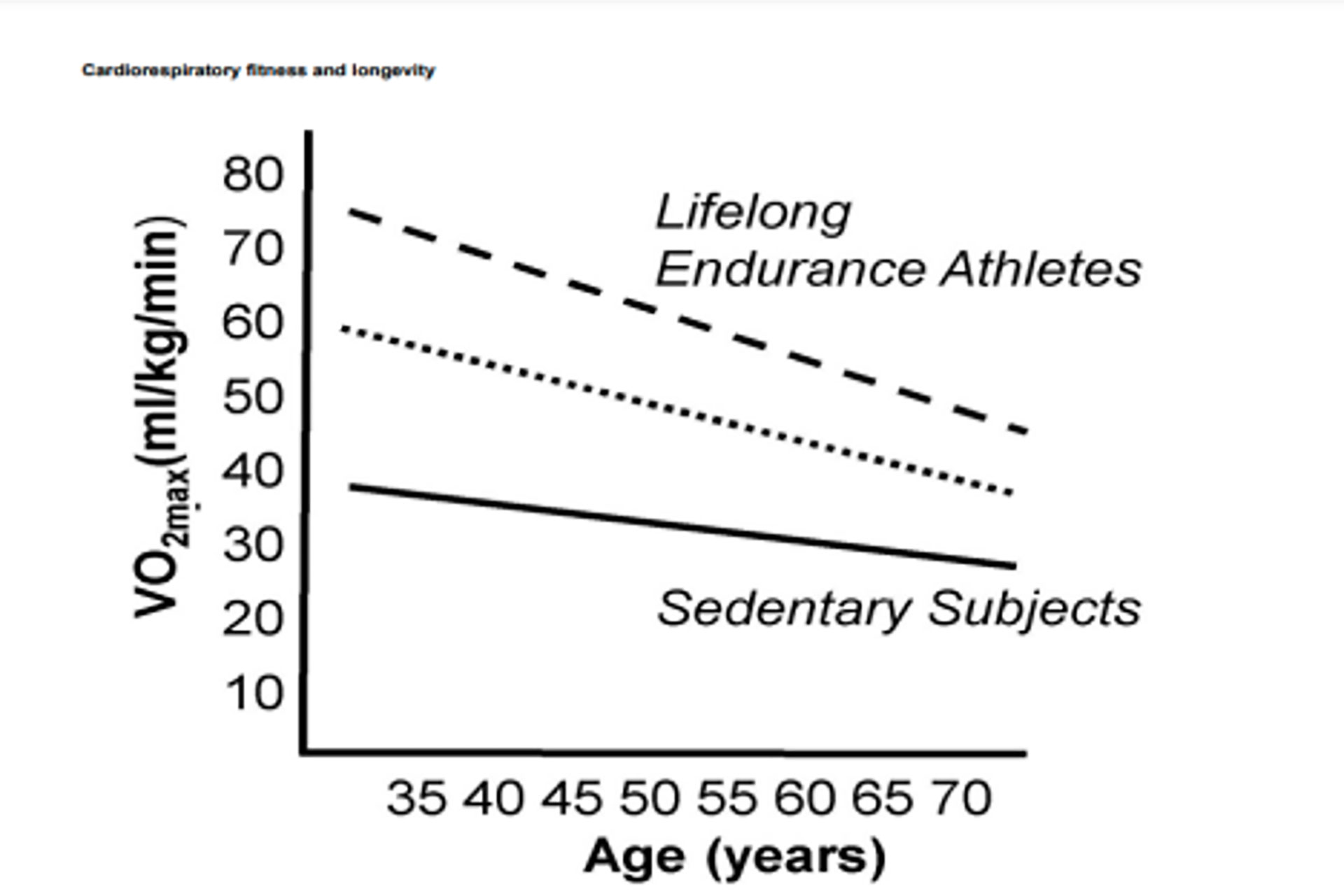
- Strength and muscle mass can begin to decline as early as age 30 — between 3–8% per decade. At age 50, these losses may exceed 40% and 15% (respectively) every decade after (1,2,3).
- Adults can lose power 1.7x faster than their strength as they age (4).
- Individuals with below-average grip strength in one study were 50% more likely to die earlier than their stronger counterparts. Researchers concluded, “muscle weakness is a serious public health concern.” (5)
What if I told you that these age-related declines in physical fitness and health are not such a sure thing as we have all been led to believe? A recent meta-analysis of 47 studies of individuals 50 and over showed after 18 weeks of strength training, the average increases in upper and lower body strength were 49% and 62%, respectively (6). Another meta-analysis observed older adults who performed full-body strength training and found that it is possible to achieve an up to 13.5% increase in lean muscle mass (7). In terms of power development, one study showed that older adults can improve their maximal muscle power by 51% after 12 weeks of explosive and ballistic resistance training (8).
This is evidence that you can still crush your fitness goals well into your 30s, 40s, 50s and beyond while mitigating pain or injury. In this article, I will debunk the myths associated with exercise and aging. I will also give you a fitness and recovery blueprint that will help you set clear training goals, train intelligently and optimize your recovery so you can build resiliency to train for a lifetime.
You’ve been lied to
Using health-related buzz words (HIIT training, circuit training, low carb, keto, vegan) or recommendations is common in popular men’s health-related articles and magazines. And they have large audiences who are prone to listening to what they say. The most popular magazines, Men’s Health and Men’s Fitness, reach an estimated 71 million readers worldwide!
However, you should be cognizant when implementing recommendations provided in these magazines and those alike. According to a study published last year, out of 160 recommendations made across several volumes by these two popular men’s health-related journals, only 38 (23.6%) were supported by available medical literature findings (9). This literature was extensively reviewed by a panel of health experts across multiple disciplines.
While I have nothing against these two magazines and acknowledge that they have incredible reach, I recommend you speak with a fitness or healthcare provider before implementing any medical interventions obtained from a magazine. At Performance Optimal Health, we pride ourselves on being teachers and scholars. That involves educating ourselves on current research and practicing what we preach so that we can be a credible resource to help you maximize your health and fitness!
The remainder of this article will serve as a blueprint for you to navigate the wild west of health and fitness in search of answers to help set you on the path of accomplishing your health and fitness goals.
Goal Setting
First stop — it’s time to set clear training goals. This means digging deeper than “tone-up” or “get back into shape.” The biggest issue with goals like this is that they aren’t specific or measurable. As a result, you have no way of knowing whether your training is really working because there was no clear goal or process from the start. A better way to set training goals for yourself requires two steps. First, use the SMART method and then describe the skills or behaviors you will need to adopt that will help you accomplish this goal.
S – Specific
M – Measurable
A – Aggressive but Attainable
R – Realistic
T – Time-orientet
When you apply this method to the vague goal of “losing weight” it turns into:
“I will lose 10-pounds a month from today. I will do this by exercising 4–5 days per week and planning my meals at the beginning of the week. I will get 7–8 hours of quality sleep by adhering to a sleep schedule and use the heat sauna once every week on my off day for recovery.”
While this goal is clearly defined, we all know that life happens. It’s one thing to write down or verbalize your goal and how you will go about it, it is another to actually follow through There will be times when you are stressed, confused, frustrated and even exhausted.
Accomplishing your goal will require a balance of self-knowledge, task knowledge and grit. You must be honest with how much you are willing to give. You must be honest with how much you actually know about what it is you’re trying to do. If you don’t, consult a professional! Lastly, you must realize that failures are merely results. Understand that accountability, consistency, effort and the ability to learn from failures is the key to accomplishing any long-term goal.
Training principles
When it comes to training, progression and overload are the name of the game. More reps, more sets, more weight, more difficult exercise variations, completing a workout in a shorter period of time (training density) are all forms of these principles. However, training is not linear. If this were the case, we would all be squatting and bench-pressing thousands of pounds by now from cumulative increases over the years. Intelligent training involves manipulating specific training variables (volume, intensity) based on training goals, experience and most importantly, your ability to recover.
Furthermore, diminished returns are inevitable when you have been training for several years. You will no longer reap the same benefits (muscle growth and strength) with the same methods you once used. If you’ve been doing the same fitness routine for the past 6 months, it’s unlikely you’re getting the desired results. Therefore, subtle variations in training methods and exercises over time are critical in keeping your body strong and resilient.
Given all this, however, more training does not always equal more results. You can only train as hard as you can recover! Training itself is a catabolic process (breaking down muscle fibers) while recovery is anabolic (improved tissue strength and resiliency). However, most people have no plan for the 23 hours they spend outside of the gym. Taking this into account, creating the right balance between exercise and recovery is a critical piece of how we approach our client’s programming at Performance.
Training program
A typical training program at Performance Optimal Health follows the R7 method created by Mike Robertson. This involves dedicating a specific amount of time to multiple fitness qualities: flexibility/mobility, dynamic movement, Corrective exercise, power, strength, conditioning and recovery. The amount of time dedicated to each component of the program depends on the client’s goals and current fitness level.
Even when considering injuries, we find a way to maximize each client’s 60-minute session incorporating all of these components. As you age, you don’t have to stop doing certain exercises, methods or trade strength training for pure cardio. In fact, the research tells us we should be doing everything we can to stay fit for life by balancing the qualities previously mentioned. Here are some examples of one of our awesome clients, Paul Steed putting this on display: