Our experts break down what you need to know about Ozempic
Our optimal health experts share their perspectives on the increasing use of weight loss medications such as Ozempic. Physical therapist Robert Mahlman and nutritionists Francine Blinten and Ashley Jerry provide insights into the effectiveness, mechanisms, and potential side effects of these medications, stressing the need for a comprehensive approach that includes diet, exercise, and medical supervision. They emphasize that while these medications can aid weight loss, they should be part of a broader strategy involving healthy lifestyle changes for sustainable results.
July 18, 2024 | Robert Mahlman, PT, DPT, OCS | Ashley Jerry, MS | Francine Blinten, CCN, CNS

1. What are your thoughts as an Optimal Health professional on the recent trend in the prescription of weight loss medication such as Ozempic?
Francine: They are quite effective, with a success rate of 7 out of 10 people achieving significant weight loss. However, as with any drug therapy, the risk-benefit ratio must be carefully considered.
Ashley: As an Optimal Health professional, it is important to approach this trend with a balanced perspective that considers both the benefits and potential risks associated with these medications. Weight loss medications like Ozempic can be beneficial for individuals who have struggled to lose weight through diet and exercise alone. Weight loss medications should not be seen as a standalone solution but rather as part of a all-inclusive approach that includes dietary changes, increased physical activity, and behavioral modifications to support long-term weight management.
2. How do these weight loss drugs work?
Francine: GLP-1 agonist inhibitors work on the brain to reduce hunger and on the stomach to slow gastric emptying which increases satiety. The drugs stimulate insulin production, which regulates blood sugar.
Ashley: Exactly. These medications work by helping to regulate appetite, increase feelings of fullness, and potentially enhance metabolic function, leading to more effective weight loss outcomes for some individuals.
3. What are other (possibly unanticipated) effects this medication has been found to have?
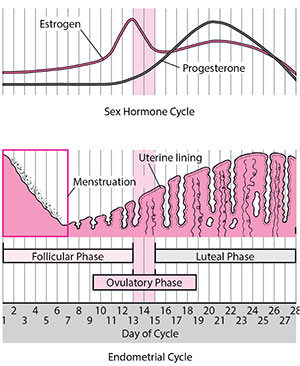
Francine: A couple of things. First, anti-addictive behavior, including reductions in cravings and altered food preferences, as well as less interest in alcohol and online shopping. It also increases fertility; there has been an increase in unplanned pregnancies for those taking the drugs. To note, the drugs are not recommended for women who are pregnant or planning to become pregnant. Other effects include muscle loss and “Ozempic face,” which can involve a sagging appearance and older-looking skin.
Ashley: They can also cause gastrointestinal issues such as nausea, diarrhea, constipation, or vomiting, as well an increased exacerbation of GERD (gastroesophageal reflux disease).
4. Do you have any concerns with the rapid increase in utilization?
Ashley: A couple of things. I am concerned about the safety of these drugs as well as the the process of monitoring of potential side effects and adverse reactions. I also ask, where are they getting these GLP-1 agonist inhibitors from? Is it a trusted source, like a physician who can monitor their health?
Additionally, each individual may respond differently to Ozempic, leading to varying experiences with both its benefits and side effects. Understanding this variability is crucial in providing personalized care and support to those considering or already using these medications for weight loss. For example, Ozempic and other drugs may alter one’s relationship with food and reduce the pleasure derived from eating, which raises concerns about the psychological impact of these medications.
Francine: These are new drugs and we still have more to learn about long term effects.
5. Do you have clients with success stories?
Francine: I’m working with several obese clients with uncontrolled diabetes who are having strong responses to the drugs such as weight loss of 15% of their body weight with improved clinical outcomes.
Ashley: I have several clients whom have had success for specifically weight loss as well as clients who have diabetes and need to lose weight for health reasons.
6. Do you have any clients who have experienced side effects and had a bad experience?
Francine: The drugs are generally well tolerated, though some experience mild nausea and fatigue. I have some clients who have switched to other GLP-1 drugs with better tolerance, for instance switching from Ozempic to Mounjaro.
Ashley: I have clients who did not lose weight on Ozempic or any other type of GLP inhibitor. Their doctor prescribed it to them specifically to control diabetes and weight, but no changes were seen. I also have had clients whom came off Ozempic because of altered mental state and increase of GERD symptoms.
7. What does the research say about weaning off these drugs once effects are seen?
Ashley: When individuals stop taking Ozempic, they may experience changes such as increased appetite, food cravings, weight gain, elevated blood sugar levels, reduced blood sugar control (especially in diabetic patients), increased blood pressure, negative changes in cholesterol levels, and mood changes related to weight regain. These effects are attributed to the normalization of physiological functions in the body after discontinuing the medication.
Experts emphasize that Ozempic is intended for long-term use and should not be abruptly stopped once desired effects are achieved. Enrolling in a nutrition program before discontinuation can help individuals make informed choices about their diet and lifestyle post-medication, ensuring a smoother transition and better management of potential side effects associated with stopping Ozempic.
8. How vital is nutrition in supporting those taking weight loss medication such as Ozempic?
Francine: The clients I see on GLP-1 agonist inhibitors have been in my care prior to starting the drugs. As such, they have made dietary improvements which serve them well as the drugs start to take effect. Nutrition support is important because as food volume decreases, the food consumed must still deliver adequate energy, macro and micronutrients.
Ashley: Sustainable weight loss requires ongoing commitment to healthy habits beyond the use of medication. Optimal Health professionals should emphasize the importance of long-term lifestyle changes to maintain weight loss results. When it comes to managing weight and overall health, the combination of proper nutrition and medication can significantly enhance the effectiveness of the treatment. Enhanced weight loss, improved metabolic health, sustained energy levels, nutrient absorption, and long term health benefits such as healthy eating habits.
9. What are other options for those looking to lose weight and avoid weight loss medication?
Robert: Adopting a balanced and nutritious diet: Focus on consuming whole foods, lean proteins, fruits, vegetables, and healthy fats while minimizing intake of processed foods and sugary beverages.
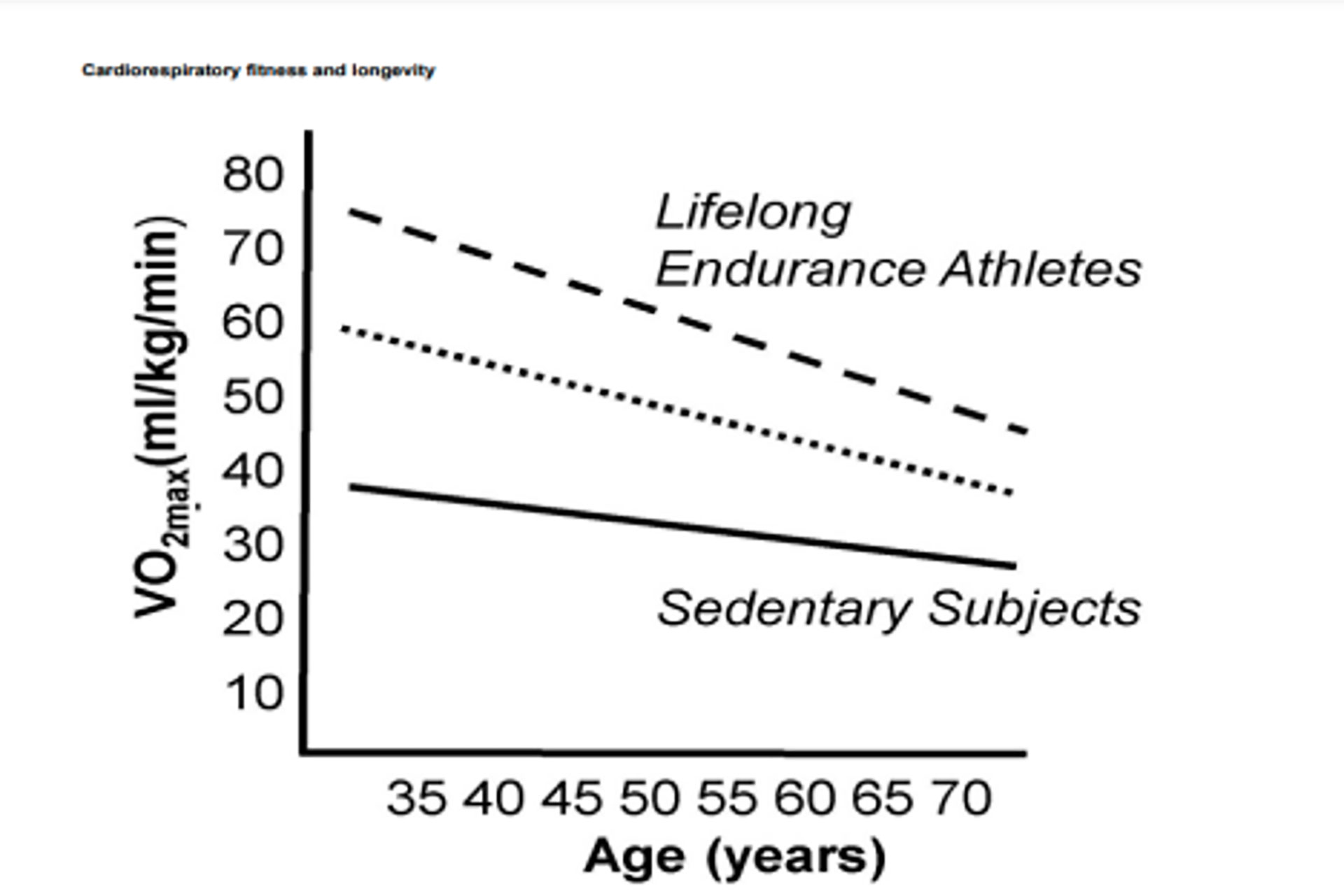
Increasing physical activity: Regular exercise, encompassing cardiovascular activities like walking, running, swimming, or cycling, alongside strength training and flexibility exercises, promotes weight loss and enhances overall health.
Seeking support: Joining a weight loss support group, collaborating with a nutritionist or dietitian, or seeking guidance from healthcare professionals can offer accountability and personalized strategies for weight loss.
Practicing mindful eating: Paying attention to hunger cues, practicing portion control, and eating slowly can prevent overeating and support weight loss goals effectively.
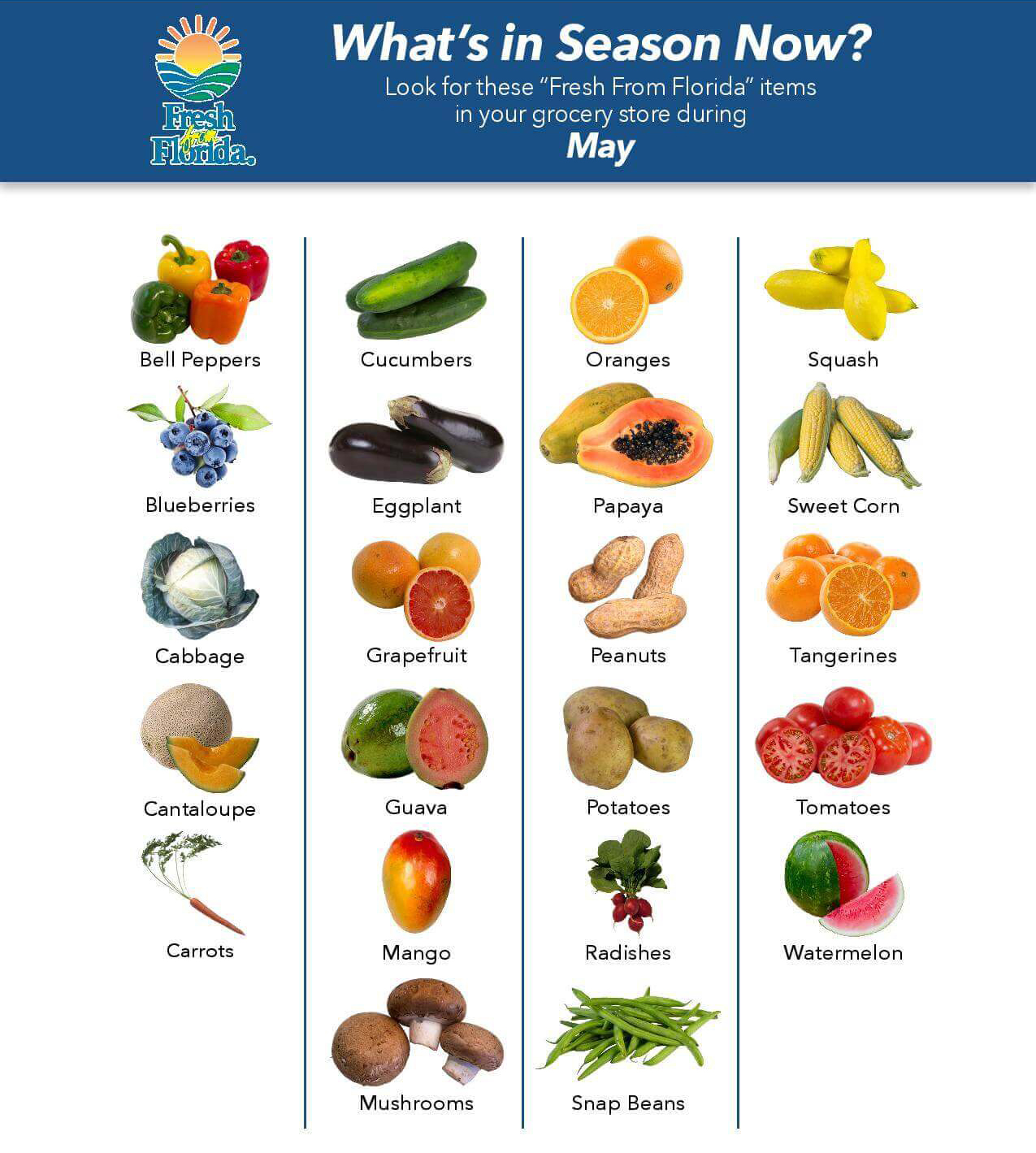
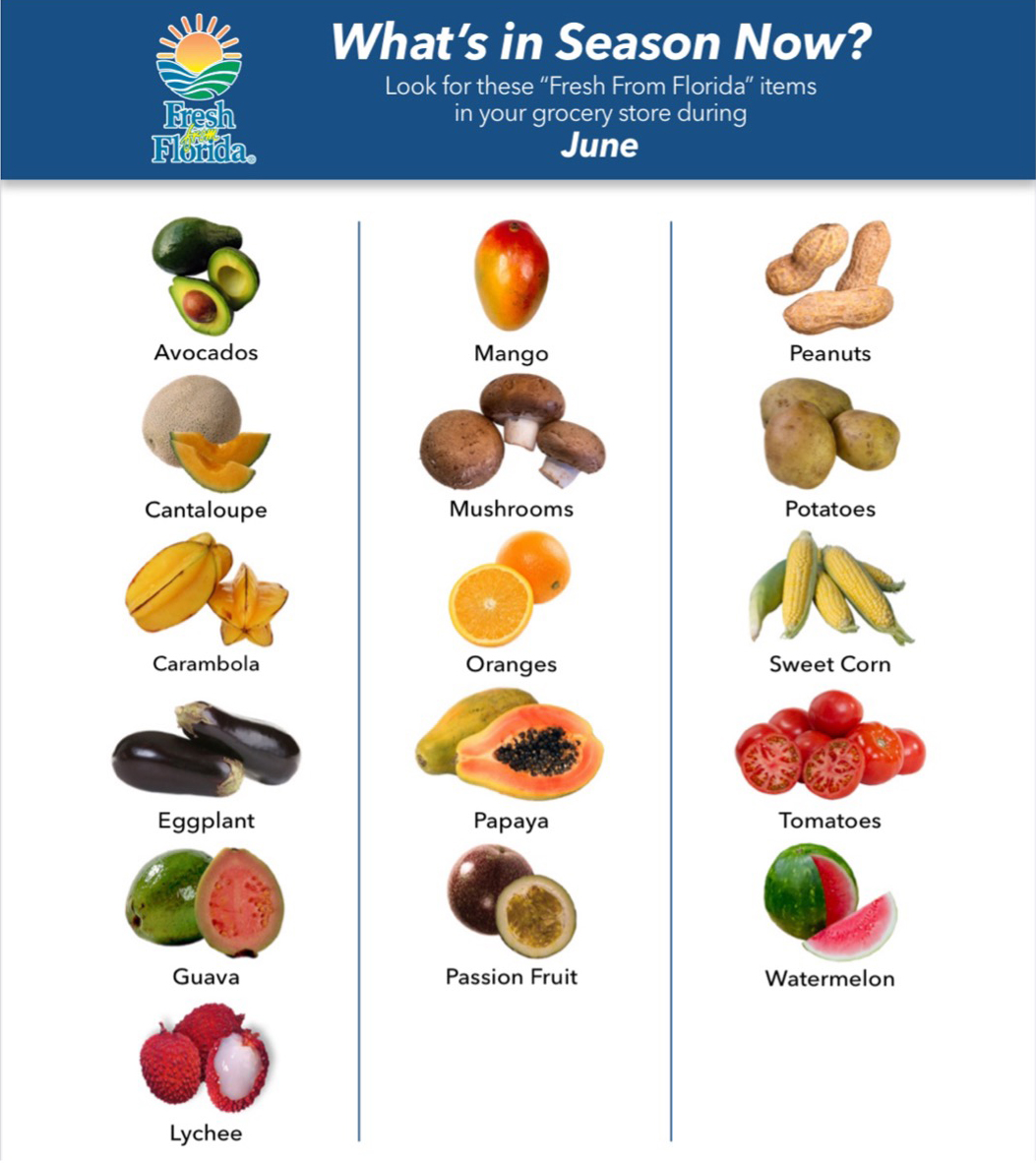
Ashley: One of the most effective ways to lose weight without relying on weight loss medication is to adopt healthy eating habits. This includes consuming a balanced diet that is rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. By focusing on nutrient-dense foods and controlling portion sizes, individuals can create a calorie deficit that promotes weight loss over time.
Making sustainable lifestyle changes can also contribute significantly to weight loss efforts. This includes getting an adequate amount of sleep each night, managing stress levels effectively, staying hydrated by drinking plenty of water, and avoiding unhealthy habits such as excessive alcohol consumption and smoking.
Behavioral modifications such as setting realistic goals, tracking food intake, identifying triggers for overeating, and practicing mindful eating techniques can enhance adherence to a healthy lifestyle and promote successful weight loss outcomes.
Francine: If the client wishes to lose weight, there are diet and lifestyle changes that can help. There is also bariatric surgery which is more invasive, but effective, in many cases.
10. How can you avoid some of the potential side effects reported with Ozempic, such as lose of bone mineral density and muscle mass?
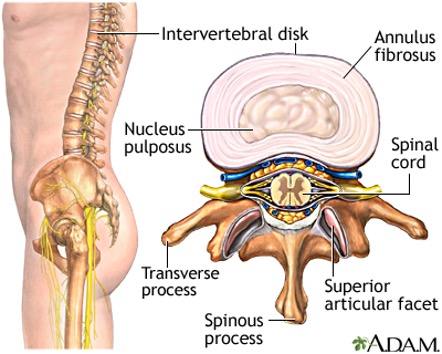
Robert: Exercise can indeed mitigate some potential side effects linked with Ozempic, such as loss of bone mineral density and muscle mass. Weight-bearing exercises such as strength training and resistance exercises aid in maintaining bone density and muscle mass. Additionally, regular exercise enhances overall bone and muscle health, thereby reducing the risk of adverse effects.
Ashley: For bone health, calcium is crucial.Foods rich in calcium include dairy products, leafy green vegetables, and fortified foods. Vitamin D helps the body absorb calcium; sources of vitamin D include fatty fish, egg yolks, and fortified foods. Protein is also essential for bone health and muscle maintenance. Good sources of protein include lean meats, poultry, eggs, fish, and beans.
For muscle mass, consuming protein-rich foods throughout the day can help maintain muscle mass. Additionally, omega-3 fatty acids have anti-inflammatory properties that may help reduce muscle breakdown. Sources of omega-3s include fatty fish, flaxseeds, and walnuts.
11. What has your experience been working with individuals on weight loss medication thus far?
Francine: It has changed the way we practice nutrition. I spend more time educating clients on portion sizes and feeding intervals, and I encourage the people in my care to keep food journals. It is interesting to compare the journal content from before treatment to the present.
Robert: My experience thus far suggests that medication is most beneficial when integrated into a comprehensive care plan rather than used in isolation. The most successful cases I've observed involved a team of healthcare professionals overseeing medication adherence, managing potential side effects, and incorporating lifestyle modifications such as diet and exercise.
12. How crucial is strength and conditioning in supporting individuals taking weight loss medication like Ozempic?
Robert: Strength and conditioning, along with exercise as a whole, should be integral components of the care plan for individuals prescribed GLP-1 agonists. It complements the effects of the medication and can significantly enhance results when performed in conjunction. From a diabetes prevention perspective, exercise assists the body in utilizing insulin more efficiently and increases cellular sensitivity to its effects. Regarding weight loss, building muscle mass through strength training can elevate metabolism and enhance calorie burning. Furthermore, conditioning exercises can enhance cardiovascular health, endurance, and overall wellness, all of which contribute to effective weight management.